When a tissue experiences inflammation, its cells remember. Pinning proteins
to its genetic material at the height of inflammation, the cells bookmark
where they left off in their last tussle. Next exposure, inflammatory memory
kicks in. The cells draw from prior experience to respond more efficiently,
even to threats that they have not encountered before. Skin heals a wound
faster if it was previously exposed to an irritant, such as a toxin or
pathogen; immune cells can attack new viruses after a vaccine has taught
them to recognize just one virus.
Now, a new study in Cell Stem Cell describes the mechanism behind
inflammatory memory, also commonly referred to as trained immunity, and
suggests that the phenomenon may be universal across diverse cell
types.
“This is happening in natural killer cells, T cells, dendritic cells from
human skin, and epidermal stem cells in mice,” says Samantha B. Larsen, a
former graduate student in the laboratory of Elaine Fuchs at The Rockefeller
University. “The similarities in mechanism are striking, and may explain the
remitting and relapsing nature of chronic inflammatory disorders in
humans.”
Uncelebrated immunity
When thinking about our immune system, we default to specific immunity—that
cadre of T cells and B cells trained, by experience or vaccination, to
remember the specific contours of the last pathogen that broke into our
bodies. But there’s a less specific strategy available to many cells, known
as trained immunity. The impact is shorter-lived, but broader in scope.
Trained immunity allows cells to respond to entirely new threats by drawing
on general memories of inflammation.
Scientists have long suspected that even cells that are not traditionally
involved in the immune response have the rudimentary ability to remember
prior insults and learn from experience. The Fuchs lab drove this point home
in a 2017 study published in Nature by demonstrating that mouse skin that
had recovered from irritation healed 2.5 times faster than normal skin when
exposed to irritation at a later date.
One explanation, the Fuchs team proposed, could be epigenetic changes to the
skin cell genome itself. During inflammation, regions of DNA that are
usually tightly coiled around histone proteins unravel to transcribe a
genetic response to the attack. Even after the dust settles, a handful of
these memory domains remain open—and changed. Some of their associated
histones have been modified since the assault, and proteins known as
transcription factors have latched onto the exposed DNA. A once naïve cell
is now raring for its next fight.
But the molecular mechanism that explained this process, and how the cell
could use it to respond to types of inflammation and injury that it had
never seen before, remained a mystery.
Inside a memory domain
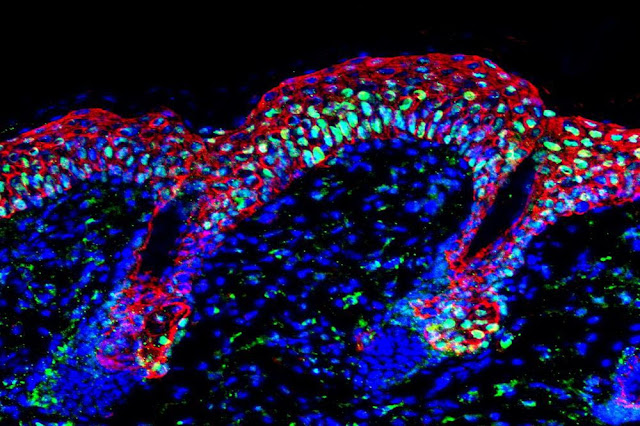
So the Fuchs lab once again exposed mice skin to irritants, and watched as
stem cells in the skin changed. “We focused on the regions in the genome
that become accessible during inflammation, and remain accessible
afterwards,” says Christopher Cowley, a graduate student in the Fuchs lab.
“We call these regions memory domains, and our goal was to explore the
factors that open them up, keep them open and reactivate them a second
time.”
They observed about 50,000 regions within the DNA of the stem cells that had
unraveled to respond to the threat, but a few months later only about 1,000
remained open and accessible, distinguishing themselves as memory domains.
Interestingly, many of these memory domains were the same regions that had
unraveled most prodigiously in the early days of skin inflammation.
The scientists dug deeper and discovered a two-step mechanism at the heart
of trained immunity. The process revolves around transcription factors,
proteins which govern the expression of genes, and hinges on the twin
transcription factors known as JUN and FOS.
The stimulus-specific STAT3 transcription factor responds first, deployed to
coordinate a genetic response to a particular genre of inflammation. This
protein hands the baton to JUN-FOS, which perches on the unspooled genetic
material to join the melee. The specific transcription factor that sounded
the original alarm will eventually return home; FOS will float away as the
tumult quiets down. But JUN stands sentinel, guarding the open memory domain
with a ragtag band of other transcription factors, waiting for its next
battle.
When irritation strikes again, JUN is ready. It rapidly recruits FOS back to
the memory domain, and the duo charges into the fray. This time, no specific
transcription factor is necessary to respond to a particular type of
inflammation and get the ball rolling. The system unilaterally activates in
response to virtually any stress—alacrity that may not always benefit the
rest of the body.
Better off forgotten
Trained immunity may sound like a boon to human health. Veteran immune cells
seem to produce broader immune responses; experienced skin cells should heal
faster when wounded.
But the same mechanism that keeps cells on high alert may instill a sort of
molecular paranoia in chronic inflammation disorders. When the Fuchs lab
examined data collected from patients who suffer from systemic sclerosis,
for instance, they found evidence that JUN may be sitting right on the
memory domains of affected cells, itching to incite an argument in response
to even the slightest disagreement.
“These arguments need not always be disagreeable, as animals benefit by
healing their wounds quickly and plants exposed to one pathogen are often
protected against others,” says Fuchs. “That said, chronic inflammatory
disorders may owe their painful existence to the ability of their cells to
remember, and to FOS and JUN, which respond universally to
stress.”
The scientists hope that shedding light on one possible cause of chronic
inflammatory disease may help researchers develop treatments for these
conditions. “The factors and pathways that we identify here could be
targeted, both in the initial disease stages and, later, during the
relapsing stages of disease,” says Cowley. Larsen adds: “Perhaps these
transcription factors could be used as a general target to inhibit the
recall of the memories that cause chronic inflammation.”
Reference:
“Establishment, maintenance, and recall of inflammatory memory” by Samantha
B. Larsen, Christopher J. Cowley, Sairaj M. Sajjath, Douglas Barrows, Yihao
Yang, Thomas S. Carroll and Elaine Fuchs, 27 July 2021, Cell Stem Cell.